Tongue tie in Adults
I have been one of the only osteopaths in Australia guiding frenectomies for the past 7 years with a functional dentists team in Brisbane. Together, we have evolved our approach to become the leaders in the field.
These take place with a wonderful team at James St Dentists which include myself, a Oral Health Therapist/orofacial myofunctional therapist and a dentist.
We are a group of female practitioners who wholeheartedly take our role seriously, with respect to each others input and professions and who work closely together to bring a caring, specific and integrated approach to addressing problems related with tongue tie.
About me:
I landed myself in this realm of tongues due to my background and interest in breathing. I have been working on my own breathing with breathwork approaches since the age of 15 which led to doing a research masters for Osteopathic Medicine in dysfunctional breathing.
Much of my continued learning has been looking at the whole person approach to dysfunctional breathing, which inspired me to begin working with newborns in the attempt to catch these dysfunctions early on and to educate as many people as I can.
I found myself working with the staff at James St dentists, mainly due to their world of knowledge but also because I cultivated a good working relationship with the practitioners and admired their functional approach.
My main interests are around sleep and breathing, and the tongue is a major player in these issues.
Why adults are questioning if they have a tongue tie:
Tongue tie has become a loud issue online. More and more people are beginning to become aware of how the position of their tongue may be implicated in their chronic issues. And they’re right to be curious!
The tongue is important on so many levels. And more predominantly, the tongue’s posture and position is important in many bodily functions and development.
People who have consulted multiple health professionals for their chronic issues are looking online to do their own research when nothing seems to be addressing the true cause.
You might be reading that an undiagnosed tongue tie may be contributing to your:
Chronic headaches
Migraines
Speech issues
Swallowing dysfunction
Sleep problems
Snoring
Chronic Fatigue
Chronic neck pain
TMD
Gut issues
Malocclusion
Cranio-facial shape
Mouth breathing
GORD / Reflux
Asthma
And this could be true for you!
Where should the tongue be sitting?
The tongue should rest gently on the roof of your palate. It should be able to sweep along the top and bottom of your teeth, all the way to the back molars.
How do I know if I have a tongue tie?
The first step towards a diagnosis is to consult with a team of professionals that have a special interest in this area. This might be an osteopath, dentist, orofacial myofunctional therapist, a speech pathologist or any other health practitioner who advertises their interest in this field.
When coming to see me at More Pathways, you will book in for an initial osteopathic consultation. During this consultation I will take a thorough health history.
The things I note during this history which may suggest to me that you have a restriction of the tongue could include:
A history of breast feeding issues (if you know your history)
Mouth breathing as a child
Unresolved jaw and neck pain
Headaches that never seem to be addressed
Unrefreshing sleep
Shoulder pain
Tension Headaches
Sleep apnea or sleep disordered breathing
Chronic issues that may include the gut or hormones
Pelvic floor dysfunction
Of course, these can be related to a myriad of other issues, but ignoring the tongue is a major mishap in approaching these problems and should always be taken into account and never missed.
Examination:
The tongue is connected to a plethora of other tissues and has far reaching connections throughout the body. This is because the body isn’t a set of seperate systems, but is truly a whole functioning unit in the truest of terms.
The frenum is not just a midline structure of connective tissue, but rather a diaphragm, tent like structure, or “skirt” that has far, structural and functional reaches.
Here is a real photograph of the tongue fascia and how far it is connected:
Examining the whole body is obviously imperative. But please take note on how closely related the diaphragm, lungs and mediastinum are.
The tongue and breathing:
The diaphragm is your breathing muscle, it sits on top of your liver and underneath your heart. It is connected directly to your ribs, sternum, heart, liver, lungs, lumbar spine, psoas muscle, eosophagus and kidneys. It has direct neural innervation from the brain and cervical (neck) spine. The eosophagus and aorta from the heart pierces through the structure. In a nutshell, it’s a very important part of your body!
When you breathe in, the diaphragm should flatten and pull the air into your lungs, when you breathe out, it should dome up and relax. The pelvic floor, from it’s various connections, should mirror this functional movement.
The diaphragm, when not functioning well, due to it’s many attachments and breathing role is a major reason why many chronic symptoms persist. Therefore, a specific examination of your breathing, with validated approaches, is important.
When the tongue is not resting on the roof of the mouth, the connections between the tongue and diaphragm don’t work well, and when that is coupled with mouth breathing (which is usually a reason or result of a low lying tongue posture) the strength and function of the diaphragm suffers.
This low lying tongue posture can obstruct the upper airway too, particularly during sleep. This has been shown to be a major reason for sleep apnea.
You can also see in the picture that the mediastinum is very close to the tongue. For this reason, examination of your ribs and shoulder girdle is also done. A high thoracic breathing pattern can lead to restrictions and tension in this area that can pull and anchor the floor of the mouth down, and further contribute to the low lying posture of the tongue and dysfunctional breathing patterns.
The tongue itself:
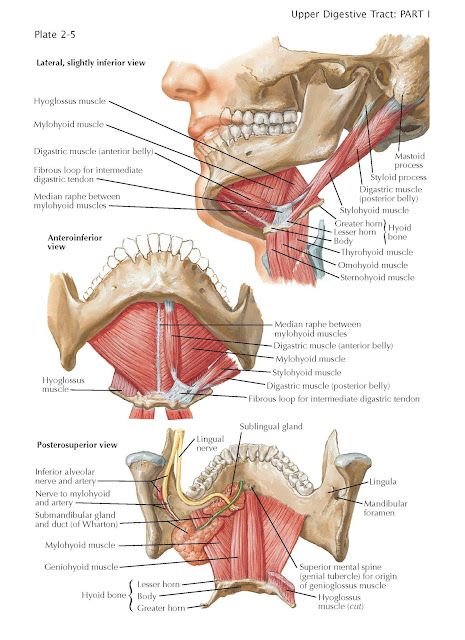
The tongue consists of 8 different muscles. The root of the tongue comes down and attaches to a bone that sits at the front of your throat called the hyoid bone. This floating bone should slide up and down and react to neck flexion and extension (nodding your head up and down). Some parts of the tongue also connect to the lower jaw bone called the mandible. Because of these attachments, these landmarks are also palpated and their movement examined during a consultation to determine any factors pertaining to tension under the tongue or a low lying tongue posture.
The tongue balances the head on the neck. The large head on such a narrow neck needs to have a strong muscular balance. With a low lying tongue posture, the head will tip down because that’s the direction of force, but because we need the eyes to look forward, the muscles at the back of the head, being the base of the skull and neck muscles, need to do extra work to pull the head back. These overworked muscles can lead to tension and headaches.
The tongue also balances the jaw. If the tongue isn’t at the roof of the mouth, it has been shown that pain and dysfunction with the jaw can arise. This is called TMD (temporomandibular dysfunction)
I also use a validated tool, called a myomate (like a little ruler) to measure how wide you can open your jaw and how high you can lift your tongue. These measurements are important in determining a true tongue tie aswell as tracking your progress with manual therapy and exercise.
Furthermore, as an osteopath, we have a particularly developed palpation that I can use in multiple ways:
Firstly, I will palpate the mucosa of the mouth, under the tongue and the frenum itself. This gives me feedback on the quality of tissue, adhesions of the fascia (a connective tissue that covers your muscle) and the muscles of the face and jaw.
We can also use this palpation to determine restrictions in the tongue/hyoid area by feeling the tissues in active movement from the neck, ribs, shoulders, sternum and diaphragm.
A special palpation is developed for the cranium …
Cranial assessment of frenulum motion:
Osteopaths are particularly trained in the bones and structures of the cranium. This is called Osteopathy in the cranial field (OCF). Cranio-sacral therapy is a derivative of this. With in-depth training, osteopaths are taught particulars of the bones of the skull, their attachments and vessel pathways along with their specific movements in relation to the rest of the body, including the fluid of the brain and spinal cord, called Cerebral spinal fluid. Osteopaths have developed a palpatory skill to determine the quality of these structures.
During an assessment, as the osteopath, I hold the bowl of the skull whilst a colleague tests the structures within the mouth, particularly the frenum, as I give feedback for the relevance of the restricted frenum and how much that tension gives feedback into the structures of the skull.
Tongue tie diagnosis:
Tongue ties in adults are multi-factorial. Often, there has been a lifetime of compensations that contribute to the tension and symptoms of a tongue tie pertaining to a multitude of manifested symptoms.
It’s imperative that a tongue tie diagnosis is conservative. Meaning, let’s not jump straight onto the frenectomy bandwagon.
Some tongues are going to be restricted because of all the above anatomic connections that could be making an impact. And it’s not only the muscles that have an effect on the function of the tongue.
The level of carbon dioxide, our breathing patterns, the nervous system, our mental health, pain and our hormones all have an effect on what our tongue does and doesn’t do and how it feels.
So, getting a well rounded, educated, approach is very important.
Your diagnosis should come from a team that works in an inter-disciplinary way and one that has mandatory protocols for pre and post frenectomy exercise and treatment.
Preparation for a frenectomy:
From a diagnosis with a professional team, the process of preparing for an informed frenectomy can begin.
Working with James St dentists, means that you will be under the guidance of an orofacial myofunctional therapist who will give you an exercise plan and goals to reach prior to release.
Given the tongues relationship to the fascia, nerves and muscles, my role osteopathically will be to address the strains in these areas and down regulate the system as well as addressing breathing patterns that may be contributing the tension in the area and system.
Breathing properly will take the load off the muscles and allow for ease and lift in the system, allowing the tongue to be less restricted and anchored whilst doing the exercises.
Functional breath work can also help balance oxygen and carbon dioxide levels, allowing rich blood perfusion to ischemic areas (if they’ve been tight a long time) and help down regulate the nervous system, allowing for a softer and more integrated recovery.
Osteopathically guided, functional frenectomy:
Now, we’re at the frenectomy itself!
I give real time feedback of the relevance of the structures that are being released by the CO2 laser, by gently holding the cranial bowl in my hands. This way, I am able to direct the dentist to release only the structures that are relevant and continue to guide the frenectomy until we find a point of ease, release and softness.
As a team, we work together as a functional whole, to maintain an approach that feels relaxing and settled for the patient.
Furthermore, osteopathically, my role is to also guide the newly released structures, now with freedom of motion they haven’t experienced before, into a gentle position in which the nervous system and body can begin it’s inherent healing work to find a midline and balance.
The dream team: Dr Natalie Moore (guiding osteopath) Dr Sylia Lee (functional dentist) Cheree Wheaton (orofacial myofunctional therapist and Oral Health Therapist)
Post frenectomy:
After the frenectomy, it’s imperative that exercises are done, laid out by the orofacial myofunctional therapist.
Now that the structures have more freedom, the work is to re-train the new found motion into it’s function, to rehabilitate the systems that had been compensating around the restrictions and to build new better habits that the tongue now has the ability to do.
There is such variation in the anatomy of the tongue from person to person, from the thickness of the frenum (there are 3 different types of frenum by the way) to the make up of the fascia, the tensile forces that create different strains in the cranium and jaw, breathing patterns, nervous system and personal experience of the patient, means there really isn’t any way to determine the outcome of a frenectomy.
Human beings and their tongues are complex and there’s many factors and layers that contribute to our experience of wellness. This is why approaching the body in a wholistic, multi dimensional way, which means, not just looking at the anatomy, but taking the biochemical and psychophysiological into account, whilst looking further than just the tongue is imperative.
The tongue really does show us the true inter-connectedness of the whole body.
Further recourses: